DSWPD may be brought on by a normal shift in the body’s internal clock that occurs during adolescence. One therapy option is to gradually move your bedtime earlier or later each night until you achieve your ideal hour.
- hp laserjet p1007 driver download for windows 7 ✓ Free Driver Download for Windows 7
- What Is Sleep Debt? 5 Tips for Catching up on Sleep
- Why Is Sleep Important For Athletes? The Connection Between Athletic Performance And Sleep
- Ultimate Guide to Choosing a Best Cooling Mattress 07/2025
- How To Sleep With Noise? Special Tips and Tricks
What is delayed sleep-wake phase disorder (DSWPD)?
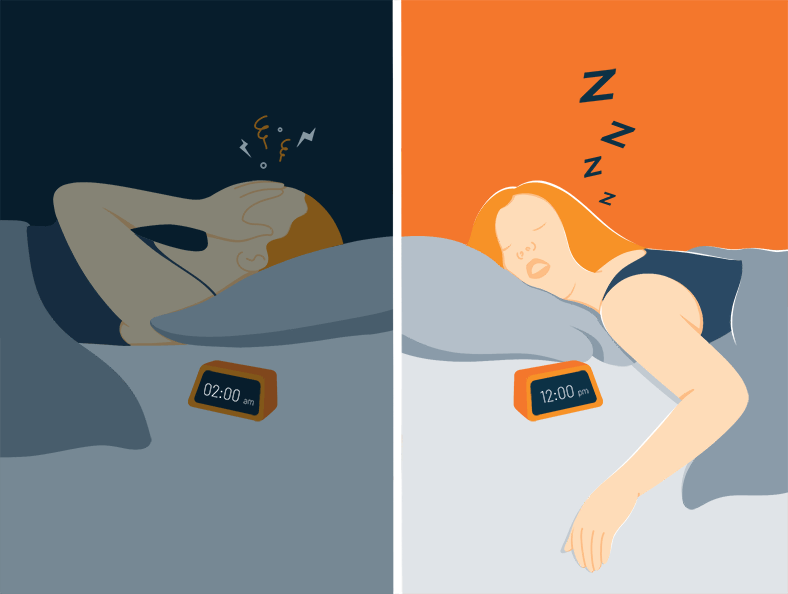
People who suffer from DSWPD have sleep that is delayed by two or more hours beyond the socially acceptable or conventional bedtime, a condition known as delayed sleep-wake phase disorder (DSWPD). Inability to wake up on time is caused by this delay in falling asleep. As an example, an adolescent with DSWPD will fall asleep long after midnight and have a tough time rising up in time for school rather than going to sleep at 10:00 pm and waking up at 6:30 am.
You are reading: Delayed Sleep-Wake Phase Syndrome (DSWPD): How To Fix It?
Adolescents with DSWPD often refer to themselves as “night owls,” claiming that this is the time of day when they are most attentive and productive. Sleep records would reveal short intervals of rest throughout the week (with few or no awakenings) and long periods of rest during the weekend (late morning to mid-afternoon wake-up timings) in the event that they were to keep one.

DSPS vs. night owl
It’s important to understand that having DSPS does not equate to being a night owl.
A night owl might stay up late to study or socialize if they are so inclined. Because of this, you’ll have to get up earlier than usual.
Your sleep schedule is flexible when you’re following an established regimen.
Staying up late isn’t an option if you suffer from DSPS. Your internal clock, on the other hand, delays sleep even if you are exhausted. As a result, it may be difficult for you to sleep and wake up at typical times.
What causes delayed sleep-wake phase disorder (DSWPD)?
Is there a known etiology for this disorder? However, between 7% and 16% of adolescents are diagnosed with DSWPD. As a result, it is a widespread condition. Psychologists suspect adolescents’ overreaction to the usual internal clock shift that occurs after puberty may be at the root of DSWPD. Despite the fact that this is not a planned act, it is crucial to note. There have been reports of DSWPD in children as young as six years old, however it is extremely rare for the disorder to emerge in early adulthood.
What are the signs and symptoms of delayed sleep-wake phase disorder (DSWPD)?
Read more : Why Is Sleep Quality Important? How Is Sleep Quality Calculated?
These are some of the signs of DSWPD
- The inability to sleep at the desired hour. Insomnia is the most common symptom. Teenagers may feel pressured to stay up late due to social norms (homework, internet or cell phone use).
- Excessive daytime sleepiness and inability to get out of bed at the desired hour. Most people complain about this since it is more obvious than nocturnal sleeplessness. DSWPD is associated with excessive daytime sleepiness in children and adolescents because of the difficulty falling asleep and the necessity of waking up on time for school or work, especially during the weekdays.
- If allowed to keep their preferred sleep/wake pattern, most people have no issues falling asleep or staying asleep. Children and adolescents with DSWPD sleep well through the night, with few or no awakenings if they are not also suffering from other sleep disorders. As a result, they are suffering from an internal shift in their sleep-wake cycle. During holidays or school breaks, children and adolescents with DSWPD tend to sleep better when there is no need to get up at a specific hour. Maintaining a good night’s rest is not a problem.
- As a result of mental health issues, Adolescents with DSWPD may experience depression as well as other psychological issues such as behavioral issues due to their inability to attend school due to excessive sleepiness during the day. The effects of daytime drowsiness on academic performance can include missed days of school, tardiness, and inattention. There may also be evidence of a dependence on caffeine, sedatives or alcohol.
Risk Groups for Delayed Sleep-Wake Phase Syndrome
Young males and middle-aged women are more likely to suffer from delayed sleep-wake phase syndrome. No substantial gender differences in DSPD have been found. Adolescents and teenagers are particularly susceptible to the condition. In the adolescent years, the body’s circadian rhythm shifts, resulting in a shift in the sleep-wake cycle. It takes kids longer to produce melatonin, the sleep hormone, as compared to adults. As a result, between 7% and 16% of teenagers are affected by DSPD. According to one study, 90 percent of persons with DSPD first show signs of the disorder in their adolescent or youth.
People with DSPD are more likely to suffer from depression than the general population. Up to 64% of those who suffer from DSPD are also depressed. ADHD may also be linked to delayed sleep phase syndrome, according to new research. Adults who were diagnosed with ADHD as children have a circadian rhythm disorder.
Diagnosis of Delayed Sleep-Wake Phase Syndrome
When it comes to diagnosing a sleep-wake phase disorder, it’s best to record your sleep patterns. You record the times you go to bed, the times you fall asleep, and the times you wake up in your sleep diary. This journal lets your doctor obtain a complete picture of your sleep patterns.
Actigraphy may also be recommended by your doctor. As if you were wearing a watch, the actigraph monitors your sleep patterns by analyzing your movement and light levels.
Diagnosing DSPD can also be done with the help of a sleep study, commonly known as a polysomnography. It is possible that you will have to take the sleep test twice. It is possible to simulate a “weekday” and a “weekend” sleep routine by taking two separate tests: These tests, however, could be prohibitively expensive.
How is delayed sleep-wake phase disorder (DSWPD) treated?
DSWPD treatment consists of the following procedures:
- Sleeping well is essential. A consistent sleep schedule and excellent sleep habits are essential for children and adolescents with DSWPD. Avoiding caffeinated products (coffee, tea, cola, some non-cola pops, energy drinks, chocolates, and some medications [Excedrin®]), as well as other stimulants and products that can disrupt sleep (alcohol, sleeping pills, nicotine), should be a part of the daily routine, as should a cool, quiet, and comfortable bedroom (computer games, smart phone, television use).
- Resetting one’s internal chronometer to a more favorable time. In this strategy, the bedtime is gradually pushed back until the target time is attained. Setting the bedtime to midnight one night, 11:45 the next, 11:30 the following, and so on, is an example of a staggered schedule.
- Reducing the speed of the body’s internal clock. The bedtime is pushed out 1 to 3 hours or more each night using this technique until the ideal bedtime is attained. It’s ideal to try this during a long school break or holiday period when people are less likely to be involved in social activities. This method is based on the belief that the body is more adaptable to a later bedtime than an early one.
- Keeping a positive outlook on the task at hand. During the holidays and weekends, it is especially crucial to keep your goals in mind. The body’s internal clock can be kept in check by strictly adhering to bed and waking hours, but this does not “fix” the propensity toward a delayed sleep-wake cycle. If you want your child or adolescent to successfully reset his or her internal clock, you must help him or her stay motivated and consistent once the appropriate bedtime has been established. After a few months of strict adherence to the program, some leeway can be granted for exceptional events alone.
- Radiant light treatment Bright light treatment is recommended by some doctors and necessitates the purchase of a specialized light box. At least 30 minutes of strong light in the morning can help reset a child’s internal clock. Reducing the amount of light in your home at night is also beneficial. It’s likely that your sleep physician has some recommendations for over-the-counter lightboxes that can help you sleep better at night.
- Medications. Some doctors may also experiment with sleep-inducing substances like melatonin or similar natural substances.
Will a teen grow out of it?
Most teens with DSPS do not outgrow it.
Read more : Multiple Sclerosis And Sleep: How Does MS Affect Sleep?
DSPS can persist into maturity, so it must be treated on a regular basis.
Your circadian rhythm will be reset during the initial treatment. However, if you want to keep the change going, you’ll need to keep going with treatment.
Your doctor will be able to advise you on the best course of treatment for DSPS.

The bottom line
Disturbance of one’s internal clock causes the syndrome of delayed sleep phase (DSPS). You can’t get to sleep until two or more hours after your “regular” bedtime because your sleep cycle is sluggish.
Being a night owl is not the same as having DSPS. Staying up late is out of the question if you have DSPS. Even when you’re exhausted, it’s impossible to sleep.
With a doctor’s guidance, you can resume a regular sleep schedule. Bright light therapy, melatonin, and proper sleep hygiene are all part of the treatment plan to help you adjust your internal clock. Adjusting your sleep and waking periods may also be necessary.
However, DSPS can occur at any age, and it is most frequent among adolescents. If you or your child are experiencing trouble sleeping, make an appointment with your doctor right once.
Please give this post a rating of 1-5 stars.
Source: https://bestpillowsleepers.com
Category: Sleep Advisors





