Metro Health Medical Center, Case Western University, Cleveland, OH, Chair Division of Gastroenterology and Hepatology; Director of the Esophageal and Swallowing Center
The IFFGD Research Award for Senior Investigator in Clinical Science was given to Dr. Fass in 2011. His other research initiatives include those aimed at improving knowledge, diagnosis, and treatment of GERD, functional heartburn, noncardiac chest pain, GERD in individuals who do not respond to PPI medication, and various investigations in patients with gastroparesis. Barrett’s esophageal patients are also being studied for the involvement of the brain in causing esophageal-related symptoms, how stroke affects patients’ symptoms, and the identification of particular markers in these patients.
GORD is the most common disease of the esophagus and a long-term chronic condition. At least 20% of the US adult population suffers from GERD-related symptoms at least once a week, according to several studies. Up to four out of five GERD patients (79 percent) report evening symptoms, according to research. Many patients with nighttime heartburn said that their symptoms interfered with their sleep, and nearly half (40 percent) noted that their symptoms hindered their ability to work the next day.
“Nighttime reflux is associated with more aggressive symptoms of GERD.”
A bi-directional association between GERD and sleep has been established in the literature. GERD has been demonstrated to disrupt sleep by arousing sufferers in the middle of the night. People with gastroesophageal reflux disease (GERD) are more likely to suffer from sleep fragmentation as a result of multiple, brief arousals. Sleep deprivation alone, however, has the potential to worsen GERD symptoms by raising the esophageal reactivity to acid and lengthening the time the acid is exposed to the esophagus.
GERD consequences such as erosive esophagitis, Barrett’s esophagus, and esophageal cancer are all linked to nighttime reflux, which is why it is so important to avoid this form of reflux. People who suffer from nighttime reflux are also more likely to experience sensations in their mouths and airways (oropharyngeal, laryngeal, and pulmonary manifestations).
GERD’s extraesophageal symptoms, such as hoarseness, throat-clearing, sore throat, wheezing, and chronic cough, have recently included poor quality of sleep and a variety of sleep disruptions. Also of major concern: Those with midnight heartburn report much lower overall health and well-being compared to those with only daytime heartburn.
Throughout the past decade, the Neuroenteric Clinical Research Group has been investigating the link between GERD and sleep in an effort to uncover its exact nature. The combination of actigraphy (a watch-like device that can tell if a patient is asleep or awake) with their pH test measuring acid exposure matched by time helped us better understand the impact of GERD on sleep. Combining the two techniques allows us to better understand how sleep and waking periods are linked to the occurrence of GERD.
The time spent in bed just before going to sleep is a vulnerable phase for gastroesophageal reflux, as we were able to show in a series of experiments that we conducted and published. The more time a person spends in bed, the more acid they are exposed to in their esophagus.
People with gastroesophageal reflux disease (GERD) were found to wake up many times during the night, according to our findings. However, only half of the awakenings were linked to gastroesophageal reflux. Most of the awakenings attributable to gastroesophageal reflux were not linked to symptoms, demonstrating that people with GERD can wake up during the night with considerable reflux but without symptoms.
After a person wakes up from a deep sleep, the majority of acid reflux incidents occur. In addition, we were able to show that waking up in the morning is also linked to a substantial amount of reflux. That is to say, for people with GERD, waking up from deep sleep is marked by severe reflux. Gastroesophageal reflux is suppressed in our research when people sleep, particularly when they sleep deeply.
One of the findings from our research was that persons with GERD need to limit the amount of time they spend in bed awake. As a result, we recently conducted a study to examine the efficacy of ramelteon (a melatonin receptor agonist), a prescription medicine that promotes sleep, on the symptoms of gastroesophageal reflux during sleep. People with gastroesophageal reflux disease (GERD) were given ramelteon prior to bedtime for six weeks, whereas a control group received a placebo. People who took ramelteon at night for six weeks reported fewer symptoms of gastroesophageal reflux disease at night. The improvement in sleep quality demonstrated by a questionnaire explains the impact.
During a recent study, we looked at the effect of napping in causing gastroesophageal reflux disease. Because of the shallower sleep that napping causes, it increases the risk of gastroesophageal reflux. In some people, eating and napping together might exacerbate gastroesophageal reflux disease (GERD).
When compared to a comparable amount of time spent sleeping at night, we found that naps were significantly more frequently linked to gastroesophageal reflux disease (GERD) and its symptoms.
For those with GERD who experience symptoms while sleeping, we plan to investigate if drugs that improve sleep will help. The combination of an anti-reflux medicine and a sleeping tablet, such as a melatonin receptor agonist, will be the focus of our research in relieving GERD symptoms.
Healthy Sleep
People with chronic illnesses like functional gastrointestinal (GI) and motility disorders need to prioritize getting enough quality sleep above all else. Your digestive system may be affected if you don’t get enough sleep. Sleep deprivation might be exacerbated by gastrointestinal (GI) symptoms. To comprehend the importance of sleep, it is helpful to have a basic understanding of sleep science. Knowing how you can enhance your sleep habits is also important.

Different Stages of Sleep
Non-rapid eye movement (NREM, stages 1–4) and rapid eye movement (REM, stage 5) sleep are the two basic states of sleep. Getting a good night’s sleep requires completing each step of the cycle.
- Stage 1: It’s a transitional state between waking and falling asleep. Muscle activity has slowed down during this period.
- Stage 2: Body temperature decreases, brain waves calm down, and respiration and heart rate remain regular throughout the second stage of sleep.
- Stage 3–4: These stages of sleep are the most restorative. The heartbeat slows, the blood pressure lowers, and muscular action halts as a result of a decrease in oxygenation. When the body’s energy is replenished and tissue is repaired, healing takes place. The release of growth and development hormones occurs at this time as well.
- Stage 5: Stage 5 is the only stage of REM sleep. Breathing becomes erratic and quick, resulting in a rapid heartbeat. Blood pressure and heart rate rise as a result. This stage allows the muscles to become even more relaxed, which gives the brain and body more energy. Dreams arise during this time. REM sleep has also been shown to boost the portion of the brain responsible for memory and learning.
Effects of Sleep
Physical, mental, and emotional health are all dependent on a sufficient amount of sleep each night. The following are a few advantages to getting enough sleep:
- Having a clear head.
- The quickness of thought and action.
- Memories are made by creating them.
- Concentrating on a single objective.
- Muscle mass growth.
- Cell and tissue regeneration.
- Boost the immune system by releasing hormones that aid in the fight against illness.
- Controlling how much energy the body uses.
- Managing the discomfort.
Tips for Improving Your Sleep Habits
A better night’s sleep is within your reach if you follow these simple suggestions. If you continue to have difficulty sleeping or if you do not feel rested during the day despite spending the night in bed, you may wish to see your doctor.
- Keep to a regular bedtime and wake-up time. Maintain a consistent sleep/wake schedule (even on weekends).
- Exercise. Make time for physical activity on a regular basis.
- Avoid consuming coffee and nicotine. Caffeine’s effects may not be fully gone for up to eight hours.
- Avoid drinking before going to sleep. You’re more groggy when you’ve had a drink.
- Late at night, stay away from heavy meals and alcoholic beverages. As a result, you may find yourself waking up frequently to go to the bathroom because of this.
- Avoid snoozing after a meal because it can promote heartburn.
- After 3 p.m., you should not be napping. Sleep deprivation is a possible side effect.
- Before going to sleep, take some time to unwind. A portion of your nightly routine should include this.
- Make sure you have a comfortable bed. Get rid of everything that might keep you awake, such as televisions, computers, bright lights, or noises.
- Keep yourself awake at night by not snoozing. Getting out of bed if you’ve been awake for more than 20 minutes is a good idea.
What Is GERD?
GERD is characterized by recurring bouts of reflux that have a negative impact on one’s quality of life.
Reflux is a condition in which stomach acid travels up the digestive tract and into the upper esophageal sphincter (LES). Reflux can occur when the muscles at the bottom of the esophagus (the so-called LES) are weak or relaxed and don’t close all the way, which is known as gastroesophageal reflux (GER).
Reflux affects nearly everyone at some point, although for the majority of individuals, it is mild, intermittent, and self-resolving.
For those who suffer from GERD, however, acid reflux occurs on a more frequent basis and with more severe and debilitating symptoms. Although it is typically associated with adults, it can also affect newborns and children.

What Are the Symptoms of GERD?
The most frequent symptom of GERD is heartburn, which causes a burning sensation in the chest, although not all instances of GERD are caused by heartburn.
Gastritis also causes regurgitation, or the passing of stomach contents into the mouth or throat, which is a common symptom of GERD.
Coughing and a sense of choking can occur when stomach acid escapes into the mouth and throat. Hoarseness and a painful throat may result from it. Dysphagia, or the sensation of something obstructing one’s throat, can occur in some people.
GERD can induce radiating chest pain that can radiate to the neck, back, jaw, or arms in addition to heartburn discomfort, and this pain can linger for minutes or hours. People with gastroesophageal reflux disease (GERD) are more likely to wake up in the night because of this sensation.
Why is GERD Worse After Going to Bed?
After going to bed, the symptoms of gastroesophageal reflux disease (GERD) tend to worsen.
- Gravity no longer aids in lowering stomach acid when lying down, making reflux more likely.
- Reduced swallowing while sleeping reduces stomach acid’s downward force.
- When you’re sleeping deeply, your saliva production decreases, which can aid to neutralize stomach acid.
As a result of a combination of these contributing factors, stomach acid leakage and retention, which may lead to more severe GERD symptoms including sleep disturbances, may be made easier. If a person goes to bed soon after eating and/or eats foods that cause GERD, the condition may be significantly worse.
What Are the Health Consequences of GERD?
There are major consequences to long-term acid reflux and GERD. Esophageal ulcers, scar tissue that restricts the passage of food, chronic cough, tooth decay, and a worsening of asthma symptoms are all indications of gastroesophageal reflux disease (GERD).
Barrett’s esophagus occurs in roughly 10% to 20% of instances of gastroesophageal reflux disease (GERD). However, not all patients with Barrett’s esophagus acquire esophageal cancer.
What Causes GERD?
Other factors have been shown to increase the risk of developing GERD, such as a weak lower esophageal muscle and a family history of the ailment.
These factors increase the likelihood of having gastroesophageal reflux disease. A person with these risk factors may or may not go on to develop GERD, and vice versa.
- Obesity: In those who are overweight or obese, GERD occurs at a higher rate, but the exact reason for this is unknown.
- Smoking Cigarettes: Tobacco smoking has been shown to alter the pressure at the lower esophageal sphincter, which could impede the elimination of stomach acid.
- Drinking Alcohol: Due to its effect on the esophageal and stomach emptying processes, alcohol can exacerbate acid reflux disease.
- Using Certain Medications: Reflux can be exacerbated by a wide range of drugs including several asthma, blood pressure, antidepressant, and sedative treatments.
- Hiatal Hernia: In this case, the stomach rises over the diaphragm and into a posture that makes reflux more likely.
- Dietary Choices: Heartburn or reflux can be brought on by a number of different foods and beverages. Chocolate, tomatoes, spicy cuisine, vinegar, citrus, fatty foods, carbonated beverages, coffee, and mint are just a few of the foods and beverages that fall into this category.
- Pregnancy: Pregnancy-related GERD is common, but it normally subsides within a few weeks of giving birth.
How Are GERD and Sleep-Related?
According to the National Sleep Foundation’s 2001 Sleep in America Poll, GERD is a common cause of insomnia. Nearly 60% of those with frequent heartburn reported that it had an effect on their sleep, and over 30% reported that it had an effect on their ability to function throughout the day.
When GERD symptoms flare up after lying down, it can be difficult to get to sleep and disturb your sleep with heartburn, chest pain, and coughing. People with gastroesophageal reflux disease (GERD) have been observed to have a worse quality of sleep in sleep clinics.
GERD and Obstructive Sleep Apnea
Obstructive sleep apnea (OSA), a sleep disorder that causes pauses in breathing during sleep, has been linked to gastroesophageal reflux disease (GERD). Opinions differ among doctors as to whether GERD is the root cause of OSA or if the two are simply linked by risk factors.
At night, it is likely that GERD causes apneas since it affects the airway and breathing abilities. OSA sufferers may also wake up frequently at night, which may lead to GERD symptoms being discovered. The esophagus may be more vulnerable to reflux as a result of OSA-induced sleep deprivation.
GERD and OSA are both associated with increased risk of alcohol intake, smoking, and obesity, hence the link between the disorders may be due to these variables.
Even though more research is needed to determine the specific link between GERD and OSA, it is obvious that the two disorders can coexist and cause substantial issues with a person’s sleep, comfort, and general health when they do.
How Can People With GERD Get Better Sleep?
Many GERD sufferers are interested in learning about ways to alleviate the condition and improve sleep quality. There is no one-size-fits-all cure for heartburn and GERD, but there are practical steps you may take to alleviate symptoms and improve the quality of your sleep.
Work With a Doctor
If you have frequent or severe GERD symptoms, difficulty sleeping, or drowsiness during the day, you should visit a doctor. A doctor is an ideal person to analyze the condition, determine the possible cause, conduct appropriate tests, and propose therapy for these complex medical issues.
When treating GERD, a doctor may choose to focus on treating the underlying problem, such as sleep apnea, in order to reduce the number of nocturnal awakenings.
Medical and non-medical treatment alternatives are available. Some of these treatments are discussed in the following sections, but a doctor is the best person to weigh the benefits and drawbacks for any given patient.
Lifestyle Changes
Managing GERD often necessitates making alterations to one’s way of life in order to eliminate or minimize the presence of triggers. Reducing one’s intake of hot and acidic foods, keeping a healthy weight, and quitting smoking are just a few examples.
Because GERD symptoms often worsen at night, several dietary and lifestyle adjustments are geared toward improving sleep quality for those with GERD.
- Avoid eating late. Reducing the risk of reflux by waiting at least three hours after a meal before going to sleep can help.
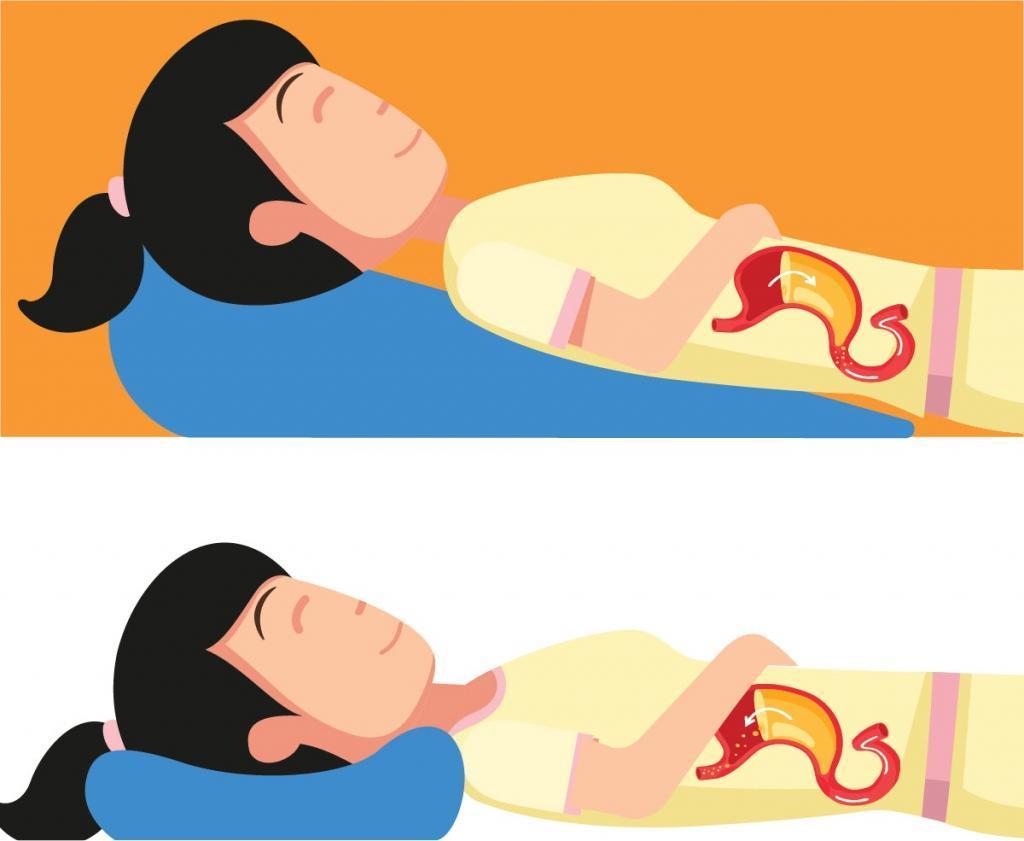
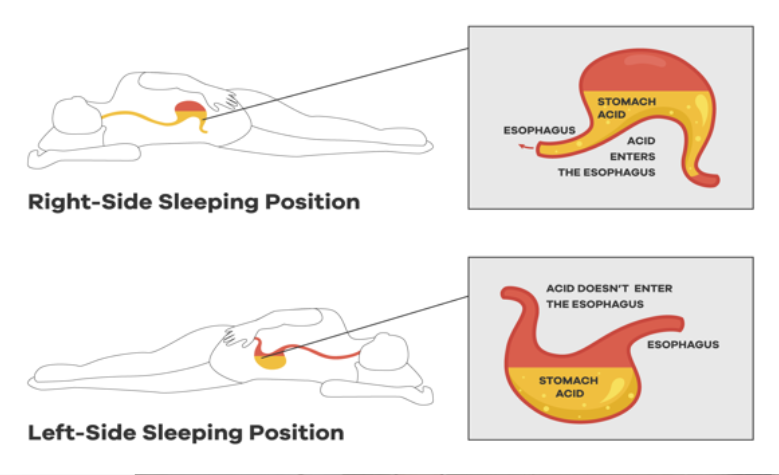
- Sleep on your left side. People with gastroesophageal reflux disease (GERD) should sleep on their left side, according to numerous studies. When you sleep on your left side, your esophagus is less likely to be exposed to stomach acid. Reflux can be worsened by sleeping in various positions, such as on your back.
- Raise the head of the bed: When you’re laying down, it’s best to raise the top of your bed at least six inches, not simply the pillows under your head. An adjustable bed frame and the best mattress for it are two simple ways to implement this change.
Medication
In certain cases, lifestyle adjustments alone are not enough to alleviate the symptoms of GERD, and medications may be required.
Antacids, for example, are available over-the-counter and can provide brief relief, but their efficacy is debatable for many people. Acid production in the stomach can be reduced using other medications such as proton pump inhibitors (PPIs) and H2 blockers (H2 antagonists). It’s advisable to check with a doctor before taking any of these medications, whether they’re over-the-counter or on a prescription.
Sometimes, when neither lifestyle changes nor drugs are working to relieve GERD symptoms, a patient’s doctor may recommend surgery.
Improve Sleep Hygiene
If you have GERD and are looking for a better night’s sleep, you may want to pay attention to your sleep hygiene, which encompasses all of the factors that influence your sleep environment and your sleep-related behaviors.
Reduce the number of times you wake up during the night by practicing good sleep hygiene. There are many sleep-related lifestyle adjustments that are also applicable to those with GERD, such as cutting back on caffeine and alcohol use. Other important aspects of good sleep hygiene include maintaining a regular sleep schedule, relaxing before-bedtime rituals, and a peaceful sleeping environment.
How to Improve Your Sleep When You Have GERD
Chronic acid reflux into the esophagus is a symptom of gastroesophageal reflux disease (GERD). This results in annoyance. Acid reflux and heartburn are common, but if you get them more than twice a week, you may have gastroesophageal reflux disease (GERD). It is possible that GERD can cause more serious health issues such as sleep disturbances if it is not treated.
GERD is a primary cause of sleep apnea in adults aged 45 to 64, according to the National Sleep Foundation (NSF). According to an NSF survey, persons in the United States who suffer from nocturnal heartburn are more likely than those who do not to experience the following sleep-related symptoms:
- insomnia
- daytime sleepiness
- restless leg syndrome
- sleep apnea
People with sleep apnea are more likely to suffer from GERD. It is possible to have sleep apnea when your breathing is either shallow or paused during sleep. A few seconds to many minutes may go between these interruptions. This might happen as many as 30 times an hour. These pauses in breathing are followed by a loud snort or choking sound, which is usually followed by a return to normal breathing.
Because it interferes with restful sleep, sleep apnea can leave you feeling groggy and drowsy during the day. It’s more often than not a long-term issue. As a result, it can have a negative impact on day-to-day functioning and make it difficult to focus on routine tasks. Screening for sleep apnea is recommended for patients with nighttime GERD symptoms, according to the National Sleep Foundation.
Coughing and choking are common GERD symptoms, and they seem to get worse while you’re lying down or trying to sleep. This overflow of acid can reach as high as your throat and larynx, which can cause you to feel like you’re coughing or gasping for air. As a result, you may wake up from a deep slumber.
There are several strategies to enhance your sleep if you’re experiencing any of these symptoms. Even if you have GERD, making small changes to your daily routine and behavior can make a big difference in your ability to obtain a good night’s sleep.
Use a sleep wedge
GERD-related sleep issues can be alleviated by sleeping on a large, specially constructed wedge-shaped pillow. Because it’s wedge-shaped, the pillow helps keep you partially upright, which in turn helps to reduce acid flow. Other sleeping positions that put pressure on the abdomen and worsen heartburn or reflux symptoms are also restricted.
Maternity shops may have sleep wedges if you can’t find them at a typical bedding store. These businesses frequently stock wedge pillows due to the prevalence of GERD among pregnant women. You can also check out medical supply stores, drugstores, and specialty sleep stores for additional options.
Incline your bed
If you lift your head by tilting your bed’s head forward, you may lessen the likelihood of acid refluxing into your throat while you sleep. Bed risers are recommended by the Cleveland Clinic. The legs of your bed are supported by little, column-like platforms that are inserted under them. They’re frequently employed to free up space for storage. The vast majority of stores selling housewares carry them.
GERD sufferers should not use risers beneath their bed’s footboard; instead, they should place them under the bed’s two top legs (the headboard end). Aim to keep your head higher than your feet at all times. Increasing the height of your bed’s headboard by six inches can be beneficial.
Wait to lie down
GERD symptoms might worsen and interfere with your sleep if you go to bed too soon after eating. Before going to bed, wait at least three to four hours after you’ve finished your last meal, according to Cleveland ClinicReliable Source. Snacks before going to bed should also be avoided.
Spend some time after supper walking your dog or taking a leisurely stroll through your neighborhood. In the event that a nighttime walk is not feasible, cleaning the dishes or folding clothes can often allow your digestive system time to begin processing your food.
Regular physical activity has been shown in studies to enhance and regulate sleep, according to a reputable source. Additionally, it aids in weight loss, which in turn lowers the symptoms of GERD. Exercise, on the other hand, naturally raises levels of adrenaline. To put it another way, exercising soon before going to bed can make it more difficult to get to sleep and stay asleep.
Another strategy to reduce reflux is to lose weight. Weight loss reduces intra-abdominal pressure, which lowers the risk of reflux.
Eat smaller, more frequent meals and stay away from foods and drinks that aggravate your symptoms, like large, heavy meals. The Mayo Clinic recommends avoiding certain foods and beverages:
- fried foods
- tomatoes
- alcohol
- coffee
- chocolate
- garlic
What’s the takeaway?
However, GERD symptoms can have a substantial impact on the quality of your sleep, but there are measures you can do to lessen those symptoms. In the event that you’re unable to sleep due to GERD, lifestyle changes such as decreasing weight may be necessary.
Some persons with gastroesophageal reflux disease (GERD) require medicinal treatment in addition to lifestyle adjustments. It’s your doctor’s job to help you design a treatment plan that’s tailored to your needs.

![Top Rated CPAP Machine Buyer’s Guide [current_date format=’m/Y’]](https://bestpillowsleepers.com/wp-content/uploads/2023/03/best-cpap-machine-img_6405d72310053-400x300.jpg)
![The 11 Best Cooling Weighted Blankets [current_date format=’m/Y’]](https://bestpillowsleepers.com/wp-content/uploads/2023/01/best-cooling-weighted-blankets-img_63d4ff15c615d-400x300.jpg)
![Ultimate Guide to Choosing a Best Cooling Mattress Pads [current_date format=’m/Y’]](https://bestpillowsleepers.com/wp-content/uploads/2023/01/best-cooling-mattress-pads-img_63c403115126b-400x300.jpg)
![Ultimate Guide to Choosing a Best Cooling Mattress [current_date format=’m/Y’]](https://bestpillowsleepers.com/wp-content/uploads/2023/01/ultimate-guide-to-choosing-a-best-cooling-mattress-img_63bcdba870d77-400x300.jpg)
![Ultimate Guide to Choosing a Best Cooling Comforters [current_date format=’m/Y’]](https://bestpillowsleepers.com/wp-content/uploads/2023/01/ultimate-guide-to-choosing-a-best-cooling-comforters-img_63bba2f5cd3ce-400x300.jpg)